Systematic Review Tools for Detecting Delirium Superimposed on Dementia (DSD)
Prepared by Abdus-Salaam Muwwakkil, Chief Quality Officer @ MemoryMD ([email protected])
Delirium that occurs in patients with dementia is referred to as delirium superimposed on dementia (DSD).
The prevalence of DSD (Delirium Superimposed on Dementia) in
- institutionalized patients from 1.4% to 70%
- community and hospital populations from 22% to 89%.
Healthcare Economics and Prevalence of DSD
DSD is associated with adverse outcomes that include accelerated cognitive and functional decline, rehospitalization, institutionalization and mortality.
It is associated with higher health care costs, worse functional outcomes, and higher mortality rates compared with patients with dementia alone.
It was estimated that 35.6 million people lived with dementia worldwide in 2010, with the prevalence expected to nearly double every 20 years, to 65 million in 2030 and 115 million in 2050.
By extrapolation based on the expected proportion of patients with dementia, up to 14 million patients will potentially experience DSD, representing a massive health care challenge.
By 2050, the number of individuals aged 65 and older in the United States with Alzheimer’s disease, the most common form of dementia, is projected to number between 11 and 16 million (~11% world population)
DSD by inference will affect millions of people worldwide especially in nursing home facilities.
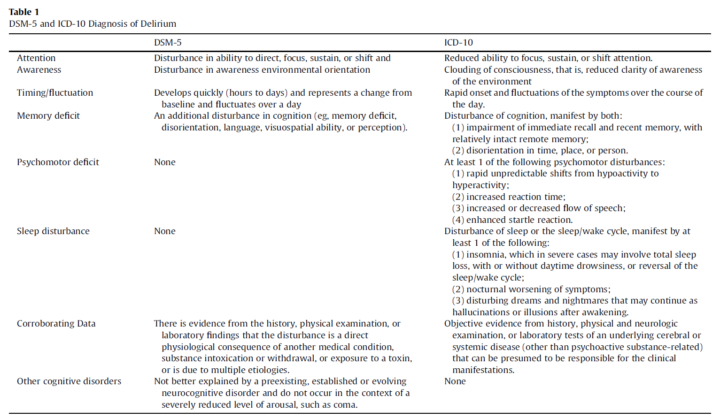
Medical Symptoms of Delirium
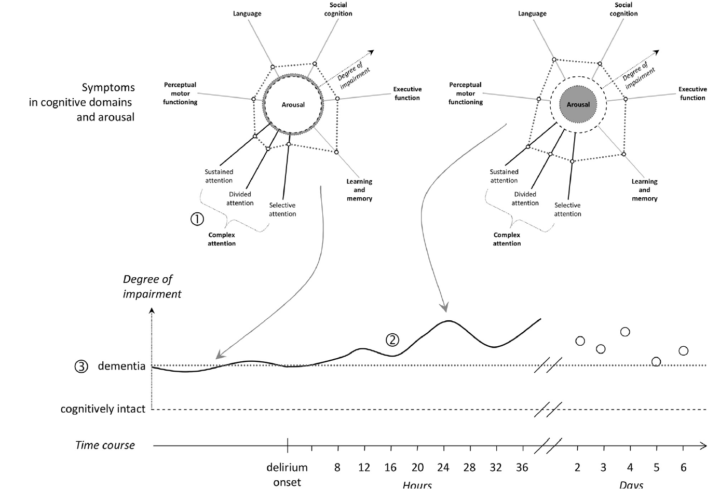
Delirium is a common geriatric syndrome characterized by acute and fluctuating disturbance
of consciousness, inattention, and deficits in arousal and cognition.
An overlap of delirium and depression might indeed interfere with the screening and
diagnosis of delirium,
Diagnostic Methods
Serial EEGs have been proposed as a useful method in the diagnosis of delirium.29
The study conducted by Thomas and colleagues28 produced mixed results:
| Sensitivity | Specificity |
| 67% | 91% |
- EEG on DSD (Thomas 2007)
- N=35
The study generalizability is limited by the exclusion of patients with severe dementia. EEG might have a place in detecting DSD research studies, though further replication in larger groups that include a greater variation in degrees of cognitive impairments is needed.
Cross Over – Alterations in level of Consciousness
Another valuable discriminating feature is level of consciousness. Alterations in level of consciousness are not always present in delirium, but when present they are highly specific to this diagnosis.
It may be that this feature is particularly valuable in situations where cognitive testing is hard to interpret due to the presence of significant underlying impairments.
Cross Over – Motor Impairment
Better descriptions of motor disturbance may also be useful, because compared to those with dementia, patients with may DSD have higher perturbation in motor agitation and retardation.
Need for Clinical Trials and Role of Objective EEG
The variation in dementia diagnostic procedures may add interpretational biases, and lead to populations with varying degrees of severity of dementia.
A formal definition of dementia obtained via neuropsychological testing, neuroimaging and biomarkers would be ideal for improving comparisons across studies.
There are currently three tools with preliminary evidence in support of their use in DSD: the CAM and the related CAM-ICU, and EEG, the latter of which lacks widespread clinical applicability. Further work is now needed to assess how these tools perform in the different stages and types of dementia, and studies with more DSD participants are required.
Additional tests such as objective assessments of attention, and examination of the discriminatory value of level of consciousness are promising areas for future study.
Works Cited
J Am Geriatr Soc. 2012 November ; 60(11): 2005–2013. doi:10.1111/j.1532-5415.2012.04199.x
Am Geriatr Soc. Author manuscript; available in PMC 2013 November 01.